
Home / Blog / Monkeypox Explained: What It Is, How It Spreads, and How to Stay Safe
Table of Contents
Over the past few days, the news about the latest Mpox or monkeypox outbreak has been all over the press – be it about the WHO announcing Mpox as a global health emergency or how our country is preparing itself for a possible outbreak.
You may have come across multiple videos, news articles, or even WhatsApp forward messages on how to protect yourself against Mpox. However, if you are confused about what to believe and what to follow, you are not the only one.
In this article, we will be discussing monkeypox symptoms, modes of monkeypox transmission, monkeypox treatment, and monkeypox prevention.
Read this blog article till the end to know the right measures that you must take to reduce your Mpox risk.
Mpox, formerly called monkeypox, is a viral infection caused by the monkeypox virus, a form of zoonotic virus that belongs to the genus Orthopoxvirus of the Poxviridae family. A zoonotic virus refers to a virus type that can spread to humans from non-human sources and vice versa.
The viruses Mpox and smallpox belong to the same family, and therefore, in some cases, a smallpox vaccine is recommended for monkeypox prevention.
Two distant clades or variants of Mpox have been identified: Clade I (formerly referred to as the Congo Basin Clade) and Clade II (formerly referred to as the West African Clade).
Clade I is further classified into Clade Ia and Ib, and Clade II is further classified into Clade IIa and IIb.
Reports suggest that infections associated with Clade II are relatively less severe than infections caused by Clade I.
For those wondering, “How did monkeypox start?” here is some brief information on when it was discovered, when the first human case was reported, and more.
In 1958, the Mpox virus was first discovered in Denmark. This virus was detected in laboratory monkeys when they started exhibiting symptoms of poxvirus transmission.
In 1970, the first human Mpox case was reported in the Democratic Republic of Congo (DRC).
In 2020, approximately 4594 suspected cases of Mpox were reported throughout the world.
In 2022, the global outbreak of Clade IIb began and multiple cases of Mpox were reported throughout the world, especially in Africa, EU countries, and the United States of America.
Between 2023 and 2024, the DRC reported the largest number of Clade I cases in one year.
In September 2023, the endemic outbreak of Clade Ib Mpox began in Kamituga, a mining town belonging to the South Kivu province of the DRC.
In 2024, between January and May, more than 4500 suspected cases of Mpox and nearly 300 deaths were reported.
Owing to the alarming surge in Mpox cases, the WHO announced this outbreak as a public health emergency of international concern (PHEIC) on August 14th, 2024.
As of August 26th, 2024, two cases of Clade Ib were reported outside Africa in Sweden and Thailand.
As of August 28th, 2024, there have been no cases reported in India.
Mpox and Smallpox belong to the genus Orthopoxvirus. Since these both viruses belong to the same genus, they exhibit similar properties, and in some cases, smallpox vaccines are administered to reduce Mpox risk. The below table elucidates the major differences between Mpox and smallpox infections:
|
Parameters |
Mpox |
Smallpox |
|
Causative Agent |
Monkeypox virus |
Variola virus |
|
Strains |
Clade I and Clade II |
Variola minor, variola major, malignant smallpox, and haemorrhagic smallpox |
|
Reservoirs |
Rodents, monkeys, and humans |
Humans |
|
Transmission |
Face-to-face contact, skin-to-skin contact, exposure to infectious lesions and body fluids, respiratory droplets, mother-to-foetus transmission. |
Face-to-face contact, skin-to-skin contact, exposure to infectious lesions and body fluids, and respiratory droplets |
|
Incubation Period (Time between exposure to virus and presentation of symptoms) |
3-21 days |
7-17 days |
|
Duration of Illness |
2-4 weeks |
5 weeks |
|
Treatment |
No standard treatment; smallpox vaccine administration is recommended to prevent Mpox. |
Smallpox vaccine |
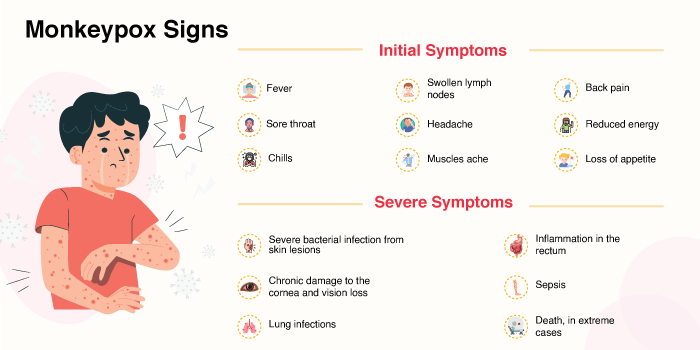
Mpox-infected individuals may experience different symptoms. Initially, individuals infected with Mpox may experience fever, chills, headaches, etc. Within a week, infected individuals develop rashes, which is a hallmark symptom of Mpox.
The severity of the symptoms experienced depends on factors like the Mpox clade, the patient’s age, and their overall health status.
The following are the monkeypox symptoms seen initially. In some cases, rashes appear as the first symptom. However, in other cases, the following symptoms may be observed initially:
Skin rash is a telltale sign of Mpox. In infected individuals, rashes start as flat sores, which within 1-2 weeks become fluid-filled blisters. These blisters can be itchy and painful and can form on different parts of the body, namely the face, mouth, throat, arms, legs, chest, genitals, and anus.
The total duration of this illness is 2-4 weeks. When the lesions dry up, crust over, and fall off, it indicates that the infection has resolved completely.
The skin rash caused by the Mpox virus progresses through different stages:
|
Stages |
Rash type |
Characteristics |
|
Stage 1 |
Macules |
Flat, discoloured spots that are round; appear within 1-2 days. |
|
Stage 2 |
Papules |
Flat spots become <1 cm bumps |
|
Stage 3 |
Vesicles |
Blisters filled with clear fluids; can be painful |
|
Stage 4 |
Pustules |
Pus-filled blisters; can be itchy and painful |
|
Stage 5 |
Scabs |
Blood crusts over the sores; skin starts healing as scabs fall off. |
Despite being a self-limiting disease, Mpox can cause severe symptoms and complications in some cases, especially if the infected individuals have compromised immunity or other underlying conditions.
The following are the potential severe symptoms and complications of the Mpox infection:
There are multiple modes of transmission for the Mpox virus. Being aware of these modes can help one take appropriate measures to reduce their Mpox infection risk.
Direct contact with infected humans and individuals showing monkeypox symptoms in the form of face-to-face contact (talking, breathing, etc.) can increase one’s risk of developing Mpox infection.
Coming in direct or indirect with body fluids, sores, and scabs found on infected individuals also increases the Mpox infection risk.
Skin-to-skin contact with the infected individuals in the form of hugging, kissing, and sexual intercourse is another way the Mpox infection spreads.
Coming into close contact with animals infected with Mpox can also cause the Mpox infection to spread.
Getting bites or scratches from infected animals and activities like playing with, hunting, cooking, and eating infected animals will increase the Mpox infection risk.
Rodents and monkeys are predominantly found to carry the Mpox virus.
While Mpox primarily spreads through close contact, there are chances of this virus spreading when healthy individuals come in contact with the objects touched by infected individuals.
Bedding, towels, doorknobs, utensils, remotes, phones, etc., are some of the objects that could cause the spreading of the Mpox virus.
While Mpox predominantly spreads through close contact. In rare cases, this virus can spread through air, dust, and surfaces too.
Those caring for infected individuals should be extra careful to not have direct or indirect contact, regularly disinfect the potential surfaces carrying viruses, and ensure that the infected individuals strictly follow the isolation protocols until the infection subsides.
The diagnosis of Mpox poses a significant challenge because its symptoms resemble those of other viral infections like chicken pox, measles, scabies, syphilis, herpes, and other sexually transmitted diseases. Therefore, a physical examination alone will not be sufficient for a Mpox diagnosis.
A polymerase chain reaction (PCR) test that detects the viral DNA in the collected sample is recommended as a preferred test for Mpox detection.
Diagnostic samples for this test include cells collected from the rash, skin, fluids, or crusts. In individuals who have not developed rashes yet, swabs from the throat or anus may be collected for the PCR test.
Blood tests are not recommended for Mpox detection.
People often search for “monkeypox treatment medicine” or “monkeypox treatment antibiotics” online. However, it is crucial to note that there is no standard treatment protocol available for Mpox at this moment.
Fortunately, Mpox is that it is a self-limiting or self-recovering disease. This infection resolves on its own without any treatment. The medical interventions recommended for Mpox infection include home isolation, supportive care, and pain management.
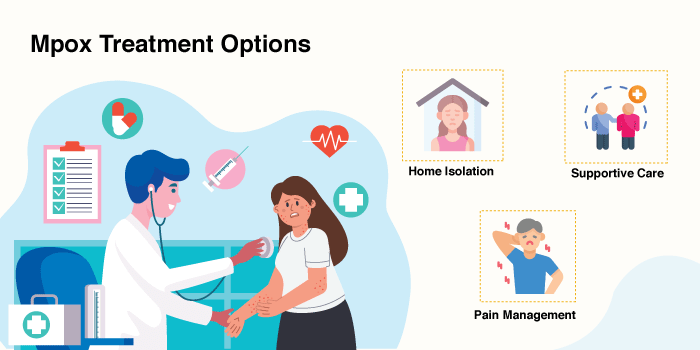
Home Isolation: One of the first things recommended for Mpox is home isolation. This measure is crucial to curbing the spread of the virus.
Supportive Care: Mpox-infected individuals should eat nutritious foods, stay hydrated, and rest sufficiently. They may also consider vitamin A supplementations for faster wound healing, especially if they have vitamin A deficiency.
There are high chances of Mpox rashes causing secondary infections. These rashes are to be managed carefully. The skin should be kept clean and dry, and rashes should not be scratched. They should be covered with breathable bandages.
Pain Management: Skin rashes caused by the Mpox virus can be itchy, painful, and cause severe discomfort. In such cases, doctors may recommend medications, such as opioids or NSAIDs, to manage pain and topical creams to reduce the dryness and itchiness of the rashes.
Currently, JYNNEOS and ACAM2000 are the two vaccines recommended by the CDC for monkeypox prevention.
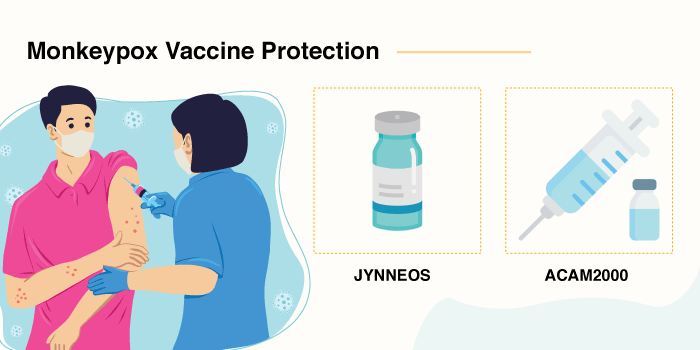
JYNNEOS: JYNNEOS is an FDA-approved live, non-replicating vaccine available for Mpox and smallpox. Two doses of this vaccine are recommended with an interval of 4 weeks between the first and second doses.
ACAM2000: ACAM2000 is another FDA-approved vaccine for smallpox, and it is synthesised using the Vaccinia virus, which belongs to the poxvirus family.
Both of these vaccines are not available in India.
Recently, the Serum Institute of India announced that it is developing a vaccine against Mpox, and it will be available within a year.
With appropriate Mpox preventive measures, you can reduce your infection risk significantly. Mpox infection is rare and can only spread when there is close contact with infected individuals and contaminated objects. The following are a few measures that you can take to reduce your Mpox infection risk:
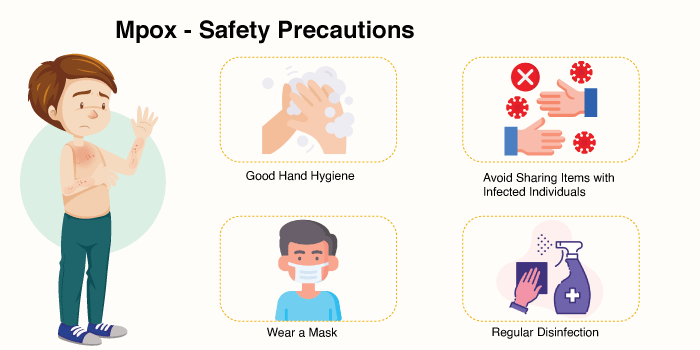
Certain personal protection measures against Mpox can help you reduce your risk of developing this infection:
To reduce your Mpox infection, you should completely avoid contact with infected individuals:
If you suspect that you or someone you know may have an Mpox infection, it is important to inform the healthcare authorities. Home isolation will be recommended where the infected individual will be isolating themselves in a room without moving around too much.
The treatment for Mpox involves supportive care, where the doctor will guide the infected individuals and their families on how to manage rashes and other symptoms caused by the infection.
Mpox is a self-limiting infectious disease caused by the monkeypox virus. This infection lasts for 2-4 weeks and can cause painful rashes, fever, swollen lymph nodes, and tiredness.
While there is no standard treatment approach available for Mpox, patients are recommended supportive care that involves the management of various symptoms, including rashes, until the infection subsides.
HCG Hospitals, a leading multispeciality hospital in India, has a robust team of infection specialists who specialise in treating and managing a broad spectrum of infectious diseases. At this moment, HCG Hospitals is awaiting further orders from the health ministry on how to ensure that the country smoothly navigates through this impending Mpox outbreak.
That said, HCG Hospitals understands that it is important to raise awareness about this outbreak among the masses and help them learn the different measures that can reduce their infection risk.
Having close contact with an infected person or animal and contaminated materials can increase the risk of Mpox infection:
Mpox is a self-limiting or self-recovering disease, i.e., it resolves on its own without any medical treatment.
There are no standard treatments available for Mpox infection. Supportive care is recommended as treatment for Mpox where symptoms are managed using different approaches and measures are taken to reduce the risk of secondary infections.
The Mpox infection lasts anywhere from 2 to 4 weeks. During this period, the rashes formed progress through various stages before completely healing.
In most cases, Mpox infection can be managed at home with supportive care. However, medical supervision is necessary in case the symptoms are severe and need to be managed with appropriate medical interventions.
Skin rashes caused by Mpox will need special attention as they can cause dry and itchy sensations, which can lead to severe discomfort. Below are a few things that infected individuals can do to manage their rashes:
Yes, there are two vaccines available for monkeypox prevention, namely JYNNEOS and ACAM2000.
At this moment, these vaccines are not available in India. The Serum Institute of India is currently developing a Mpox vaccine, which may be available by next year.
An individual may take 5–21 days to develop symptoms after being exposed to the Mpox virus.
Yes, Mpox infection can be transmitted through sexual contact.
The Mpox vaccine is expected to offer protection against the infection for at least two years, according to reports by the CDC. Booster doses may be required depending on exposure risk.
If you are experiencing the symptoms of Mpox infection, it is important to isolate yourself and inform the medical authorities immediately. It is important to not come into close contact with healthy individuals to prevent the infection from spreading.
You must take care of your rashes and lesions by cleaning them properly and covering them. It is also important to eat healthy, stay hydrated, and rest well.
The rashes will heal within four weeks. In most cases, patients recover with supportive care. However, if the symptoms are severe and unmanageable, one must see a doctor.